The CBRPC and Drs. Aatur Singhi, David Geller and Paul Monga were integral contributors to the collaborative publication by Torok etal. entitled, “Matrix viscoelasticity promotes liver cancer progression in the pre-cirrhotic liver”.
Fan W, Adebowale K, Váncza L, Li Y, Rabbi MF, Kunimoto K, Chen D, Mozes G, Chiu DK, Li Y, Tao J, Wei Y, Adeniji N, Brunsing RL, Dhanasekaran R, Singhi A, Geller D, Lo SH, Hodgson L, Engleman EG, Charville GW, Charu V, Monga SP, Kim T, Wells RG, Chaudhuri O, Török NJ. Matrix viscoelasticity promotes liver cancer progression in the pre-cirrhotic liver. Nature. 2024 Jan 31. doi: 10.1038/s41586-023-06991-9. Epub ahead of print. PMID: 38297127 .https://rdcu.be/dxSJu
ABSTRACT:
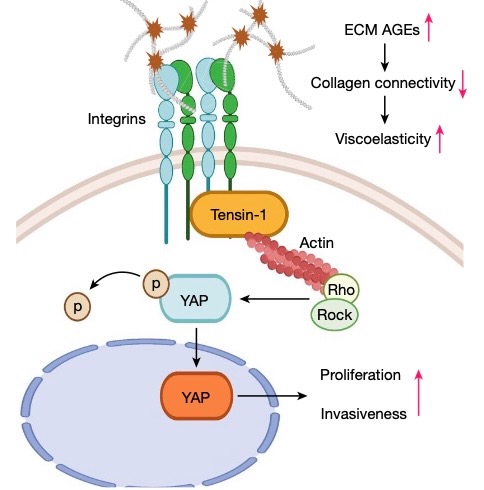
Type 2 diabetes mellitus is a major risk factor for hepatocellular carcinoma (HCC). Changes in extracellular matrix (ECM) mechanics contribute to cancer development1,2, and increased stiffness is known to promote HCC progression in cirrhotic conditions3,4. Type 2 diabetes mellitus is characterized by an accumulation of advanced glycation end-products (AGEs) in the ECM; however, how this affects HCC in non-cirrhotic conditions is unclear. Here we find that, in patients and animal models, AGEs promote changes in collagen architecture and enhance ECM viscoelasticity, with greater viscous dissipation and faster stress relaxation, but not changes in stiffness. High AGEs and viscoelasticity combined with oncogenic β-catenin signalling promote HCC induction, whereas inhibiting AGE production, reconstituting the AGE clearance receptor AGER1 or breaking AGE-mediated collagen cross-links reduces viscoelasticity and HCC growth. Matrix analysis and computational modelling demonstrate that lower interconnectivity of AGE-bundled collagen matrix, marked by shorter fibre length and greater heterogeneity, enhances viscoelasticity. Mechanistically, animal studies and 3D cell cultures show that enhanced viscoelasticity promotes HCC cell proliferation and invasion through an integrin-β1–tensin-1–YAP mechanotransductive pathway. These results reveal that AGE-mediated structural changes enhance ECM viscoelasticity, and that viscoelasticity can promote cancer progression in vivo, independent of stiffness